Sleep Information Page
Contents
Introduction
Research shows that between 40 and 80% of autistic children and young adults have sleep problems. They have difficulty falling asleep, staying asleep, waking very early – or all of the above!
Encouraging your child to have a good sleep pattern can be difficult, and don’t underestimate the hard work that is needed to improve things. This Sleep Information pack has been designed to help.
In this pack, you will find some general sleep hygiene advice, but also more specific interventions that recognise the additional difficulties autistic children, young people and those with special needs have.
The pack also includes some helpful websites that give great advice.

1. Creating a bedtime routine
Creating a bedtime routine is very important, and that’s why it is the first piece of advice in this pack.
Having a bedtime routine in place is not only beneficial for your child but those involved in the bedtime routine. All children and family dynamics are different so create a routine that meets your family’s individual needs with achievable goals.
To help create your own bedtime routine, here are some questions to ask yourself:
- Where do you want your child to sleep?
- What time would you like them to go to bed?
- What time would you like them to get up?
- Sleep goal?
Helpful hints
Sometimes, a routine would be better kept short and simple—dinner, TV, bath, teeth, and bed. However, for autistic children and those with ADHD or special needs, using visual pictures with time gives more structure and understanding, which may help. The key thing is to persevere. If something doesn’t work, make tweaks, but keep going.
If you are introducing a new routine, make it easy. Sometimes, it is best to start with the last thing you want them to do and work backwards (this is called ‘Backward chaining’ used in various situations).
2. Enviroment
The sleeping environment is another key factor in aiding a better night’s sleep.
- · Tidy the room for sleeping so there are fewer distractions
- · If possible, reduce the amount of furniture or clutter in the room
- · Try and use the room/area where sleep is expected to only be used for that purpose
- · Ensure everything that is needed - blanket, cuddly toy, etc is readily available
- · Create a pictorial timetable to structure the bedtime routine- this sometimes takes the pressure of parents constantly telling a child to do something. Autistic Children generally respond better to visual reminders than the spoken word.

Removing screens/TVs from children at bedtime is sometimes difficult as this may be the only thing that enables your child to sit quietly. If you are unable to stop their use due to it triggering behavioural difficulties (dysregulation), try the following suggestions:
- · create a time limit for screen use
- · watch relaxing programmes instead of playing video games or high energy films – these cause stopping sleepiness.
- · melatonin, the sleep hormone, is produced naturally to enable sleep, blue light (the type that comes from light bulbs and screens) stops melatonin from being produced and working, therefore, switching to red light bulbs and red screen filters ensures that melatonin can do its job.
3. Science of sleep
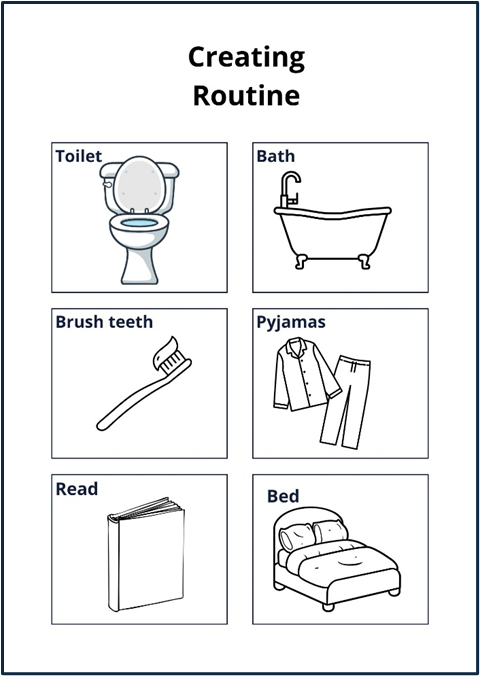
Hypnogram graph
The above graph shows a hypnogram of sleep cycle in a healthy young adult. Normal sleep involves cycling through Non Rapid Eye Movement (NREM) and Rapid Eye Movement (REM) sleep, beginning with stage 1 through to stage 4, followed by REM sleep.
Given the right circumstances, all humans follow a basic pattern during sleep. Shown in the above graph called a Hypnogram.
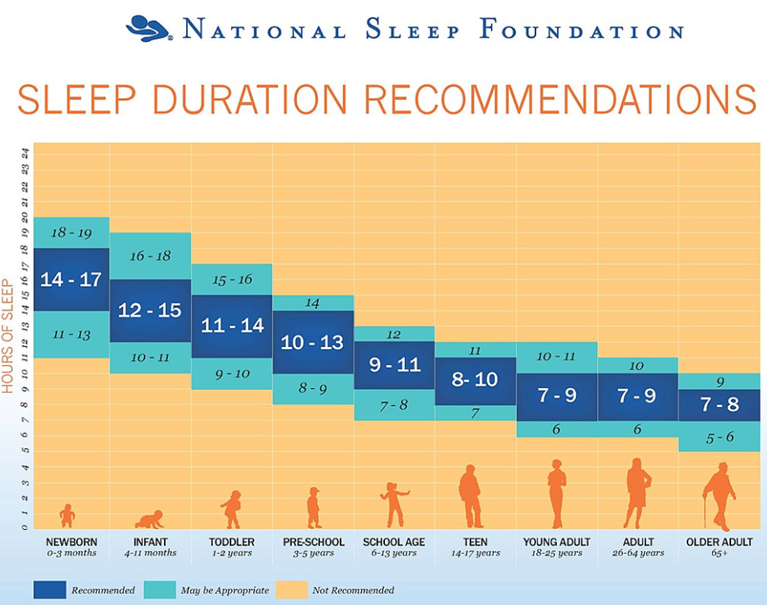
The 4 stages of sleep are detailed below. The average length of time we need to sleep is relative to our age.
Stage 1
A person moves from being awake to sleep. Lowers heart rate, breathing & muscles relax.
Stage 2
Muscles relax more, eye movement stops and body temperature drops.
Stage 3
Deep sleep is the hardest to be woken from. Heart rate, breathing and brain waves become regular. This happens mostly in the first part of the night, this decreases with age.
Stage 4
Refers to eye movement- quickly from side to side. Breathing quickens, blood pressure and heart rate are less regular. Dreams occur. During this time there is temporary muscle paralysis.
These stages happen multiple times throughout sleep. All are important for restful sleep and impact how we feel the next day.
Sleep Duration Recommendations
There are many different types of sleep disorders that children can suffer from:
- · night terrors (usually happens in first 2-3 hours of sleep, child cannot be calmed and has no memory of it afterwards)
- · parasomnia (aggressive motor behaviour during sleep)
- · sleepwalking
- · sleep apnoea (unable to breath in sleep due to upper airway collapsing, snoring occurs)
- · restless leg syndrome - an uncomfortable sensation in the legs with an urge to move, this is worse during the night and gets better with movement.
All of these can be distressing and may require additional specialist support. If you are concerned about any of these, please speak to your GP or consultant.
4. Toileting

One of the most common problems alongside sleep for autistic children and those with special needs is toileting. Wetting the bed and constipation are the key things that will interrupt a night’s sleep.
Bedwetting (also referred to as Enuresis)
Children up to the age of 7 are prone to bedwetting incidents. If your child continues with these difficulties after the age of 7 you may want to arrange a visit to a health care professional for further investigation.
Reduce the amount of fluid your child drinks in the 2 hours before bedtime. Fluids like squash or any fizzy drink should be avoided from lunchtime.
Constipation
Often children will hold in their poo and not want to go whilst at school or on the toilet. If this is the case, then your child might become constipated. If your child is finding it very hard to pass poo or hasn’t had a poo in 2-3 days, then visit a healthcare professional, as an assessment is recommended.
Your child might be holding in their poo and wait until they are in bed to go in a nappy or in their bed where they may feel more comfortable and relaxed, but discomfort may wake them in the night or early morning and affect their sleep. This is something that can be addressed and often, when sorted, will also improve sleep issues. Please speak to your health care professional about this and you can find information Constipation :: Frimley HealthierTogether website.
5. Sleep diaries
Sleep Diaries are necessary for sleep assessment and review. There are so many ways to improve sleep, but it is important to know and understand how a person sleeps or doesn’t sleep to understand their needs and improve things.
A sleep diary is usually completed for two weeks and either completed by yourself or your child if they are able. There are a variety of sleep diary formats that can be used; however, in general, they are asking for the same information.
- · Naps taken and for how long
- · What time did your child go to bed?
- · What time did your child go to sleep?
- · The time of any night waking, what they did, how you responded and resettle time
- · What time did they wake up and what woke them?
- · When did they get out of bed to start the day?
- · Rating sleep from poor to very good
- · Any additions, e.g., room temperature, medication, unwell child, etc.
Sleep diaries can form part of a broader sleep assessment. Assessments will collect a complete picture of your child’s development and medical history, including any diagnosis, allergies and medication. It will also include sleeping arrangements and household set-up.
Sleep diaries are important for reviewing sleep programmes' progress and medication. If your child is involved in a sleep study, you will be asked to complete one before any appointments, allowing you to see if there have been any changes, positive or otherwise.
6, Medication for Sleep

Often with sleep difficulty people think sleep medication will help, and sometimes in the short term it might, but it does not help with long-term issues.
Sleeping medication comes in various forms. Hypnotics is very rarely used on children.
Melatonin
Melatonin is a synthetic hormone that helps with sleep onset and is the medication most prescribed.
To understand why, people's brains naturally produce the hormone melatonin at night. Melatonin may help a person go to sleep, but it does not guarantee continuous sleep.
Synthetic Melatonin, also known as Circadin (crushable tablets and liquid) and Slentyo (slow-release tablets), is given to people to induce sleep.
There has been some research to show that autistic children and those with ADHD do not produce enough Melatonin naturally, making falling asleep difficult. Studies also show that taking Melatonin increases sleep by between 22 and 57 minutes per night.
If melatonin is overused, it can lose its effectiveness as the person can become desensitised to it, and although rare, it can also have side effects, headaches, nausea, next-day drowsiness and worsening insomnia.
Children should not be on medication for the long term unless it is regularly reviewed every 6 months.
Any medication prescribed for sleep must be used alongside a regular sleep programme to encourage restful sleep. Good sleep programmes have the best results.
7. Parents are important too
Parenting a child with additional needs is challenging. Add to that a lack of sleep, and parents' stress levels will be extra high. Parents often struggle to sleep themselves, even after their child has eventually gone to sleep. In order to improve their child's sleep, it helps if parents try and remain calm and look after themselves.
Parent groups are a good opportunity to talk with others in the same situation. This is a proven way to support and inform people who are going through particular difficulties and helps them realise they are not alone.
Lack of sleep and stress can lead to further mental health issues. Please contact your GP or healthcare provider for additional support if you feel your mental health is being affected significantly.
Techniques
Many techniques for relaxation and mindfulness are available to help. Have a look at Mind which has some excellent advice.
Deep breathing – take 10 deep breaths in through your nose, and out through your mouth.
Do a body scan. Move your attention slowly from the tips of your toes up to the top of your head. Focusing on how each part of your body feels. Is it warm, tingly, tense etc? relaxing each part as you go.
Remember you need to look after yourself in order to look after others. If there is a short time in the day that you can devote to YOU, take it.
8. Helpful Websites
Home :: Frimley HealthierTogether
Constipation :: Frimley HealthierTogether
Cerebra.org.uk/sleep-advice-service
The children’s sleep charity.org.uk
Reference
The Southampton Sleep Disorder service
Figure 1: Hypnogram of sleep cycle in a healthy young adult. Adapted from Lin VW, Cardenas DD, Cutter NC, et al. Spinal Cord Medicine: Principles and Practice. New York: Demos Medical Publishing; 2003.
Figure 2 Sleep Duration Recommendations. Hirshkowitz M, The National Sleep Foundations sleep time duration recommendations: methodology and results summary, Sleep Health (2015)